Bone function and bone metabolism

Our body has a skeleton formed by about 200 bones. In addition to supporting the body, bones have a variety of functions. Bones, once made, don’t seem to change afterwards, but they are always renewed. Cells called “osteoclasts” melt and destroy old bones. (This is called “bone resorption”)
| Function | Role |
| Support function | The skeleton supports the weight of various organs of the body. |
| Motor function | Exercise with the movable joint as a fulcrum via the tendon. |
| Protection function | Protects soft (weak) organs such as brain and heart. |
| Hematopoietic function | The bone marrow (red bone marrow) produces blood cells such as red blood cells and white blood cells. |
| Storage function | Stores minerals such as calcium and sodium and releases them into the blood as needed. |
The bone forming cells called “osteoblasts” adhere to the broken part, and the bone matrix such as collagen is synthesized and calcified to form new bone. (This is called “bone formation”). Over a period of about 3 years, the whole body bones are replaced with new ones.
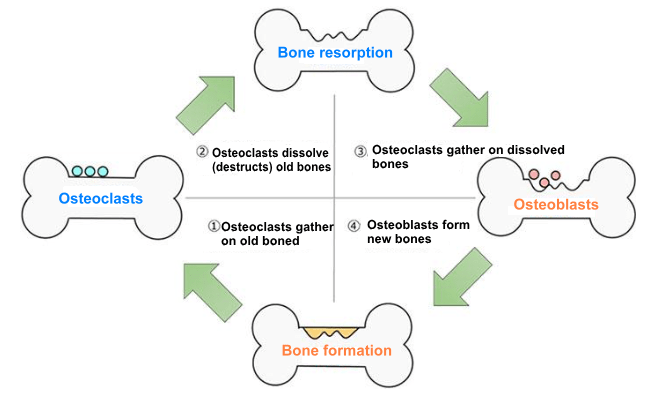
This cycle is called “bone metabolism (remodeling)”, and healthy bones can be maintained by maintaining a balance between bone resorption and bone formation.
About osteoporosis

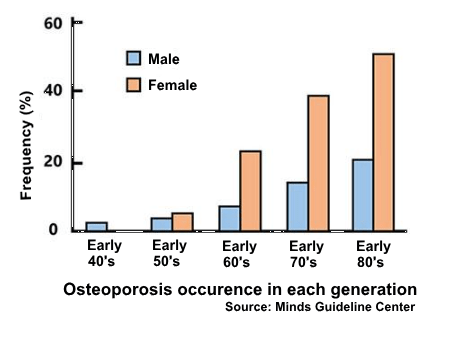
“Osteoporosis” is a disease in which bone mass and density are reduced, making the bones brittle or weak. In general, the risk of osteoporosis increases with age, especially in women. In this disease, bone weakening increases the risk of a broken bone. It is the most common reason for a broken bone among the elderly.
When osteoporosis occurs, not only pains such as fractures and skeletal deformation, but also height shortens and the center of gravity of the body shifts, making it easier a human to fall and fracture.
In addition, compression fractures due to osteoporosis greatly affect the activities of daily living, such as bent backs with decreased volume of the abdominal cavity, resulting in reduced cardiopulmonary function.
Healthy bone has a balance between bone formation and bone resorption. However, it does not regulate bone metabolism, such as parathyroid hormone (bone resorption promoting hormone), calcitonin (bone resorption inhibiting hormone), and female hormone estrogen (a hormone that promotes bone formation and suppresses bone resorption). When hormonal balance is disrupted, osteoporosis is caused because of the imbalance between bone formation and bone resorption, and osteoclasts, which destroy bones, work predominantly.
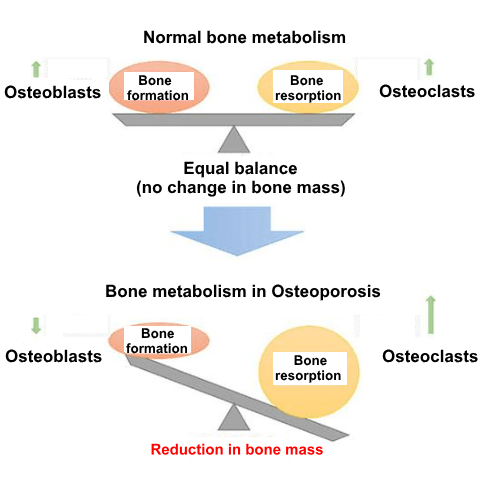
Elderly women have a higher incidence of osteoporosis because, after menopause, the secretion of female hormones (estrogens) is drastically reduced, the secretion of bone resorption-promoting hormones is increased, and the function of osteoclasts is enhanced. Thus, osteoporosis is closely related to hormone balance.
Here, is introduction of a study on the effects of Asaigermanium on “bone metabolism” by Asai Germanium Research Institute.
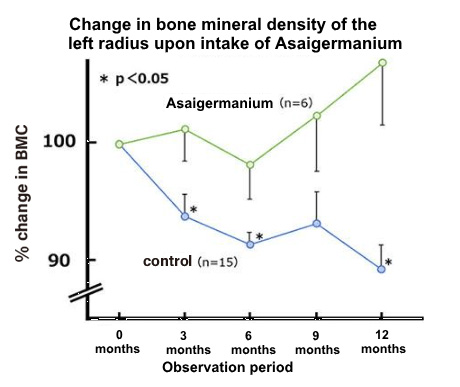
Changes in left radial bone mineral content of senile osteoporosis patients
Clinical Trial① Clinical trial of Asaigermanium for senile osteoporosis
Test:
6 out of 21 patients with senile osteoporosis, took 1500 mg of Asigermanium daily for 12 months. Bone mineral content of the left radius (bone from elbow to wrist) was observed on 0 month (before intake), and 3, 6, 9, and 12 months after the intake.
Result:
Bone mineral density in the left radius of patients who did not take Asaigermanium gradually decreased during the 12-month observation period, whereas patients who took Asaigermanium, the decrease of bone mineral density was significantly suppressed.
In addition, subsequent clinical studies have shown that small amount of Asaigermanium also achieve similar effects.
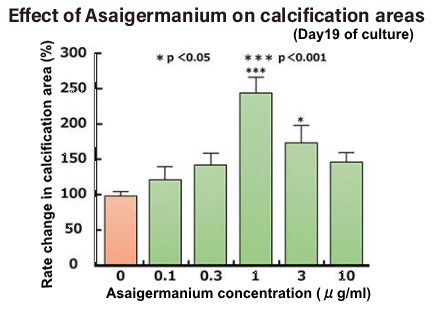
Effects on bone formation
Experiment ①Experiment on differentiation of bone marrow cells into osteoblasts and promotion of bone calcification
Bone marrow has stem cells that can become cells of any organ, and osteoblasts are also formed by differentiation and development from these stem cells. In this study, Asai Germanium Research Institute examined the effects of Asaigermanium on the differentiation of rat bone marrow stromal cells into osteoblasts and on calcification.
Test:
The bone marrow cells collected from the rat are cultured in a culture solution for 7 to 10 days to increase the number of cells, and the cells are then aliquoted into a test dish containing Asaigermanium (0.1 to 10 μg / ml) and cultured for 30 days. did. In the process, the area of calcification was examined over time.
Result:
The calcified area increased after 16 days of culture in both the Asaigermanium-added group and the non-added group. On the 19th and 30th days of the culture, compared with the group without added Asaigermanium, the added group was found to significantly increase the area of calcification, indicating calcium deposits in the bone.
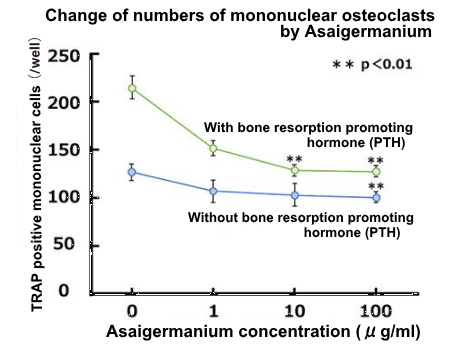
Effects on osteoclast formation
Experiment ②Effect on osteoclast differentiation
Test:
Bone marrow stromal cells were removed from the femur and tibia of a 6 weeks-old mouse into a Petri dish and cultured for 7-10 days. After that, the cultured cells are removed, then cultured for 8 days in the presence of mouse bone marrow-derived osteoblasts called ST2 cells, and stained osteoclast by TRAP staining method and count stained osteoclasts (TRAP positive cells).
Result-1:
Osteoclast precursors (immature osteoclasts without bone resorption) differentiate into mononuclear osteoclasts and then fuse to mature into multinucleated giant cells. First, when mononuclear osteoclasts were stained and counted, number of osteoclasts (mononuclear cells) increased in the group with bone resorption-promoting hormone (PTH) compared to the group without bone resorption-promoting hormone (PTH). However, the adding Asaigermanium resulted in a concentration-dependent decrease in the number of mononuclear osteoclasts, with or without bone resorption-promoting hormone.
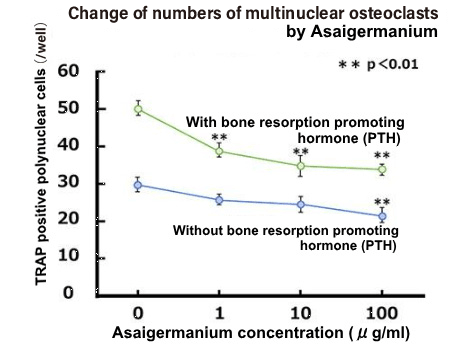
Result-2:
The number of multinucleated osteoclasts was similarly evaluated. Similar to the result-1, the group to which bone resorption promoting hormone (PTH) was added, increased the number of osteoclasts (multinuclear cells) compared to the group to which bone resorption hormone was not added. However, the adding of Asaigermanium significantly suppressed the formation of mature multinuclear osteoclasts in a concentration-dependent manner, with or without bone resorption-promoting hormone.
Intake of Asaigermanium was found to suppress the formation of osteoclasts.
Osteoporosis and Asaigermanium
As a result, “suppression of decrease in bone mineral density” was obtained in the clinical trials in human body. Also in the fundamental research, stimulation of bone calcification and differentiation to osteoblasts from myeloid cells were shown, on other hand suppression of osteoclasts formation were shown. Therefore, it is thought that the result of the fundamental research is to prove the clinical trials.
References
- Junto Ogawa “Sarcopenia and Bone Metabolism Disorder-Involvement of Muscle Loss by Aging” (in Japanese) Experimental Medicine 2014, 32 (7): 158-163
- Hajime Orimo, Takashi Akiguchi “Effects of Ge-132 on senile osteoporosis” (in Japanese) Journal of Medicine and Pharmaceutical Science 1983, 9 (5): 1507-1509
- Akihiko Wakatsuki “Case Primary Care (Emergency) Osteoporosis” (in Japanese) Japanese Obstetrical & Gynecological Society 2006, 58 (3): “N-27”-“N31”
- Fujii, A., Kuboyama, N., Yamane J., Nakao, S., & Furukawa, Y., Effect of Organic Germanium Compund (Ge-132) on experimental oseteoporosis in rats., General Pharmacology , 1993, 24 (6 ): 1527-1532
- Edited by Takuo Fujita, “Bone Metabolism and QOL -Bone and Daily Life-” (in Japanese) Medicine and Drug Journal
- Nakao Ishida and Ikuro Kimura, supervised, “Science of Organic Germanium” (in Japanese), “Toyo Igakusha”
- Okano Kazutoshi, “From the Origin of Osteoporosis to Treatment and Management” (in Japanese), Shinko Medical Publishing Co., Ltd.
- Katayama Yoshio, “ Hematopoietic environment and bone metabolism ” (in Japanese) Experimental Medicine 2014, 32 (7) ( 64-69)
- Satoru Naito, Chizuko Iwane, Takuyuki Katabami, Nobuhiko Saito “2. Effect of the organic germanium derivative Ge-132 on osteoclast formation” (in Japanese) Kanagawa Ca, Bone Metabolism 2002, 23: 9-12